MHS Access Request Form
Requirements and Instructions
Please read the following detailed instructions on how to complete our electronic form. You will not be able to print the form until all required fields are completed. Failure to fill out the form correctly will result in a delay of account creation. All three (3) pages of the form are required to process your application. Once complete, fax to the number provided at the top of the form. The link to the form itself can be found at the bottom of this page. Handwritten forms will not be accepted and you will be asked to resubmit.
Please allow a minimum of 7-10 business days after submission for access to be granted.
Click Here for the Access Request Form
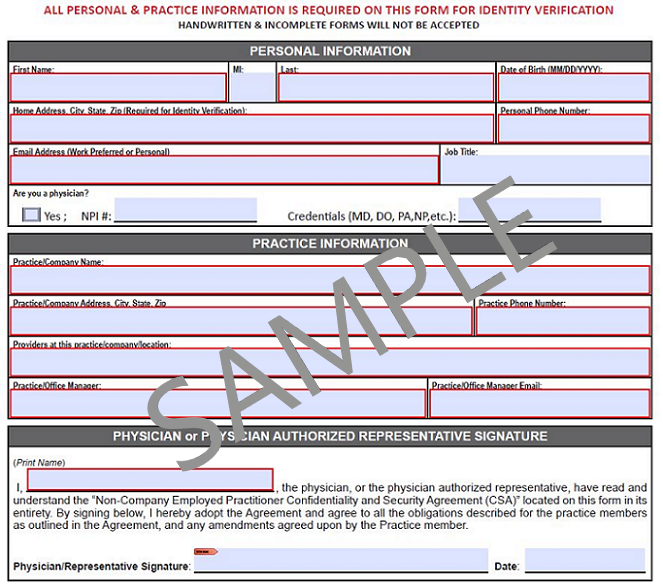
Required Fields for Printing: Fields marked highlighted in Red must be fully completed in order to gain access to Methodist/STRIC applications.
EXAMPLE FORM:
Required Fields for Processing
- Personal and Practice Information
- All personal and practice information is required for identity verification
- List physician group (practice) if applicable
- List specific Insurance Group if applicable
- Physician or Physician Authorized Representative Signature and Date
- You must have physician or physician authorized representative sponsorship to gain access to Medical Records. The physician or physician authorized representative must sign and date before faxing. Billing groups must also have a physician sponsor. (Please note, access to Meditech requires that the physician sponsor be a credentialed member of the Methodist Medical Staff)
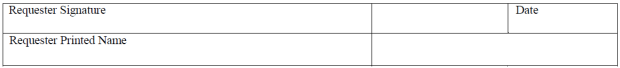
- Confidentiality and Security Agreement (CSA)
- In order to obtain access, the user must print name, sign, and date the bottom of the CSA on page 3. The customer requesting access needs to sign this section.
Why is my personal information and date of birth required?
- All personal and practice information is required for identity verification
- By law (the HIPAA Security Rule) HCA must have a mechanism to uniquely identify users with access to electronic Protected Health Information (ePHI), and verify their access and activities are necessary and appropriate through periodic reviews, activity monitoring, and audits.
- HCA must have a mechanism to uniquely identify each user on our network for government, law enforcement, and civil/legal discovery requests for logs and evidence of activities.
- HCA also must have a unique identifier to correlate network user access with other key business processes such as background checks, the OIG List of Excluded Individuals/Entities, reports on disclosure of PHI, screening for terminated workforce members, and credentialing.
- Please contact us at 210-575-0090 if you would like to receive full documentation on this requirement.